At the start of week 4, I returned to work but did not last long on ward rounds.
I now know this to be the start of long COVID.
I was breathing fast, but what also felt like breathing through a straw.
He had expected to see a mucky-looking chest X-ray, and when this came back clear, he chalked my symptoms up to either long COVID, anxiety, or reflux.“Despite a differential of long COVID, I was treated like an anxious little girl; my concerns were not taken seriously despite me being a doctor myself.I experienced episodes of altered consciousness and sleep apnea.
My body would wake me from sleep or the edge of sleep and, after a slip-second pause, I would gasp for breath.
It was at this time that I experienced a sense of impending doom, which I can only describe as an emotion felt as a physical sensation in the chest, dragging you down and pulling you under.
My sleep became disturbed.I felt a mental, physical, and emotional exhaustion like no other, but the virus or my body’s response to it kept me wide awake.
After 72 hours without sleep, I experienced external auditory hallucinations secondary to insomnia.Throughout January, February, and March, my right cerebral hemisphere felt numb and inflamed.The pain felt much deeper than that of a bacterial ear infection, like a “hot poker” sensation deep in my ear.
Although my sleep continued to be disturbed, these hallucinations were not secondary to sleep deprivation.
When I was fortunate enough to sleep, I experienced night terrors; vivid, disturbing dreams.”.
Subsequent episodes of mood and speech disturbance — which caused slowness, stammering, slurring, and more than usual word-finding difficulty, although I’ve had that, too — I believe were misdiagnosed and misinterpreted by the long COVID care team.
Throughout April, May, and June, my brain no longer felt inflamed, but it didn’t feel right.When I touched my head, the right side felt different to the left.
It physically feels like something is amiss on a cellular level, the mitochondria are not functioning properly.Even now, 1,500 healthcare worker deaths later, according to former Secretary of Health Matt Hancock, and with 122,000 healthcare workers off with long COVID, the national guidance on PPE remains unchanged.Like others with long COVID, I still experience a myriad of other symptoms — every few days I have a sore throat, sneezing, visual disturbances such as speckled vision, blurred vision, or increased floaters, intermittent diarrhea, and the rest.“I know I am carrying a lot of trauma surrounding my experience of long COVID, its impact on my body, and a string of poor medical encounters.I fear that the severity and prevalence of long COVID have been downplayed.I share my story in the hope of raising awareness about long COVID and its impact.
While waiting for treatment, many people with long COVID continue to suffer and feel forgotten.
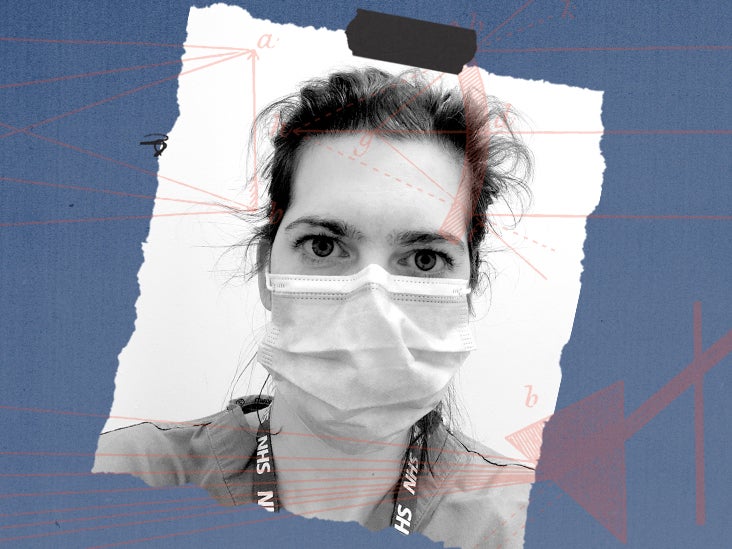
As part of our 'COVID-19, 1 year on' series, Amy Murnan writes a Through My Eyes perspective about her experience of living with long COVID for 1 yearMy name is Chris Ricketts, and last year, I experienced a life changing spinal injury