– Neurology research can include information involving brain research, neurological disorders, medicine, brain cancer, peripheral nervous systems, central nervous systems, nerve damage, brain tumors, seizures, neurosurgery, electrophysiology, BMI, brain injuries, paralysis and spinal cord treatments.
Summary: SARS_CoV_2, the virus responsible for COVID-19 infects and replicates in astrocytes, reducing neural viability.A Brazilian study published in the journal PNAS describes some of the effects infection by SARS-CoV-2 can have on the central nervous system.A preliminary version (not yet peer-reviewed) posted in 2020 was one of the first to show that the virus that causes COVID-19 can infect brain cells, especially astrocytes.Astrocytes are the most abundant central nervous system cells.Infection of astrocytes was confirmed by experiments using brain tissue from 26 patients who died of COVID-19.“For example, we can insert one antibody into the sample to turn the astrocytes red on binding to them, another to mark the SARS-CoV-2 spike protein by making it green, and a third to highlight the virus’s double-stranded RNA, which only appears during replication, by turning it magenta,” Martins-de-Souza explained.Alterations suggesting possible damage to the central nervous system were also found in these five samples.
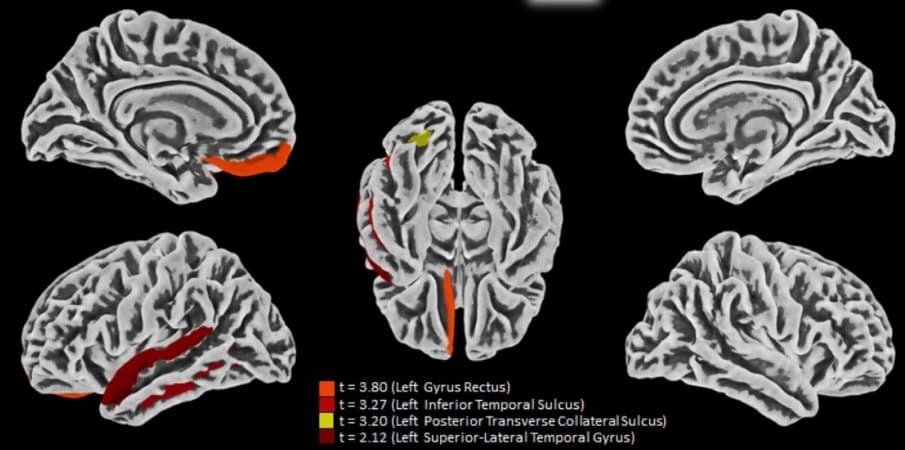
The capacity of SARS-CoV-2 to infect brain tissue and its preference for astrocytes were confirmed by Adriano Sebolella and his group at FMRP-USP using the method of brain-derived slice cultures, an experimental model in which human brain tissue obtained during surgery to treat neurological diseases such as drug-refractory epilepsy, for example, is cultured in vitro and infected with the virus.In another part of the research, conducted in UNICAMP’s School of Medical Sciences (FCM), 81 volunteers who had recovered from mild COVID-19 were submitted to magnetic resonance imaging (MRI) scans of their brains.In IB-UNICAMP’s Neuroproteomics Laboratory, which is headed by Martins-de-Souza, experiments were performed on brain tissue cells from people who died of COVID-19 and astrocytes cultured in vitro to find out how infection by SARS-CoV-2 affects nervous system cells from the biochemical standpoint.The astrocytes were obtained from induced pluripotent stem cells (iPSCs).
Martins-de-Souza’s team then used chemical stimuli to make the iPSCs differentiate into neural stem cells and eventually into astrocytes.
Results of experiments on hamsters conducted at the Institute of Biosciences (IB-USP), for example, reinforce the hypothesis that infection by SARS-CoV-2 accelerates astrocyte metabolism and increases the consumption of molecules used to generate energy, such as glucose and the amino acid glutamine.One of the discoveries revealed by the PNAS article is that the virus does not use the protein ACE-2 to invade central nervous system cells, as it does in the lungs.At UNICAMP’s Neuroproteomics Laboratory, Martins-de-Souza analyzed nerve cells and others affected by COVID-19, such as adipocytes, immune system cells and gastrointestinal cells, to see how the infection altered the proteome.“We’re also comparing the proteomic differences observed in brain tissue from patients who died of COVID-19 with proteomic differences we’ve found over the years in patients with schizophrenia.The aim of the study is to find out whether infection by SARS-CoV-2 can lead to degeneration of the white matter in the brain, made up mainly of glial cells (astrocytes and microglia) and axons (extensions of neurons).“Morphological, cellular, and molecular basis of brain infection in COVID-19 patients” by Fernanda Crunfli et al
Morphological, cellular, and molecular basis of brain infection in COVID-19 patientsWe show the spectrum of cerebral impact of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, ranging from long-term alterations in mildly infected individuals (orbitofrontal cortical atrophy, neurocognitive impairment, excessive fatigue and anxiety symptoms) to severe acute damage confirmed in brain tissue samples extracted from the orbitofrontal region (via endonasal transethmoidal access) from individuals who died of COVID-19In an independent cohort of 26 individuals who died of COVID-19, we used histopathological signs of brain damage as a guide for possible SARS-CoV-2 brain infection and found that among the 5 individuals who exhibited those signs, all of them had genetic material of the virus in the brain
Brain tissue samples from these five patients also exhibited foci of SARS-CoV-2 infection and replication, particularly in astrocytesSupporting the hypothesis of astrocyte infection, neural stem cell–derived human astrocytes in vitro are susceptible to SARS-CoV-2 infection through a noncanonical mechanism that involves spike–NRP1 interactionOur data support the model in which SARS-CoV-2 reaches the brain, infects astrocytes, and consequently, leads to neuronal death or dysfunction